What is Depression?
Overview
Depression can be described as trying to navigate daily life with dark sunglasses on. For some people, it feels like a heaviness stays with you throughout the day, making it extremely challenging to carry out what you might previously have considered simple tasks, such as getting out of bed or taking a shower. For others, it comes in waves, hitting a person repeatedly after brief periods of respite.
Sometimes, a depressive episode is triggered by a significant event like the loss of a loved one or a major life transition. However, it can also seem to come out of nowhere, even when life is seemingly continuing as usual.
Depression is not the same as the feeling of intense sadness. Rather, it is a health condition with physical and psychological roots, with sadness being one of many symptoms, which is why simply ‘getting over it’ is not possible.
Whether or not you can pinpoint the trigger of your depressive episode, and regardless of its severity, you do not have to deal with it alone. With professional treatment, including therapy, you can get the expert help you need to begin your recovery journey.
In this guide, we will explore the definition of depression, along with the types of depression, symptoms of depression, and the different treatments for depression.
What is Depression?
Depression is a mental health condition characterized by depressed mood and a difficulty experiencing pleasure, among other symptoms. It impedes a person’s ability to function as normal, in their personal, social, and work lives.
Millions of Americans are diagnosed with depression every year, making it one of the most common mental illnesses. With treatment and resources becoming more readily available in the twenty-first century, a person who receives a depression diagnosis is increasingly likely to seek and receive effective treatment. Nonetheless, there are still limitations in access to treatment, especially for underserved demographics.
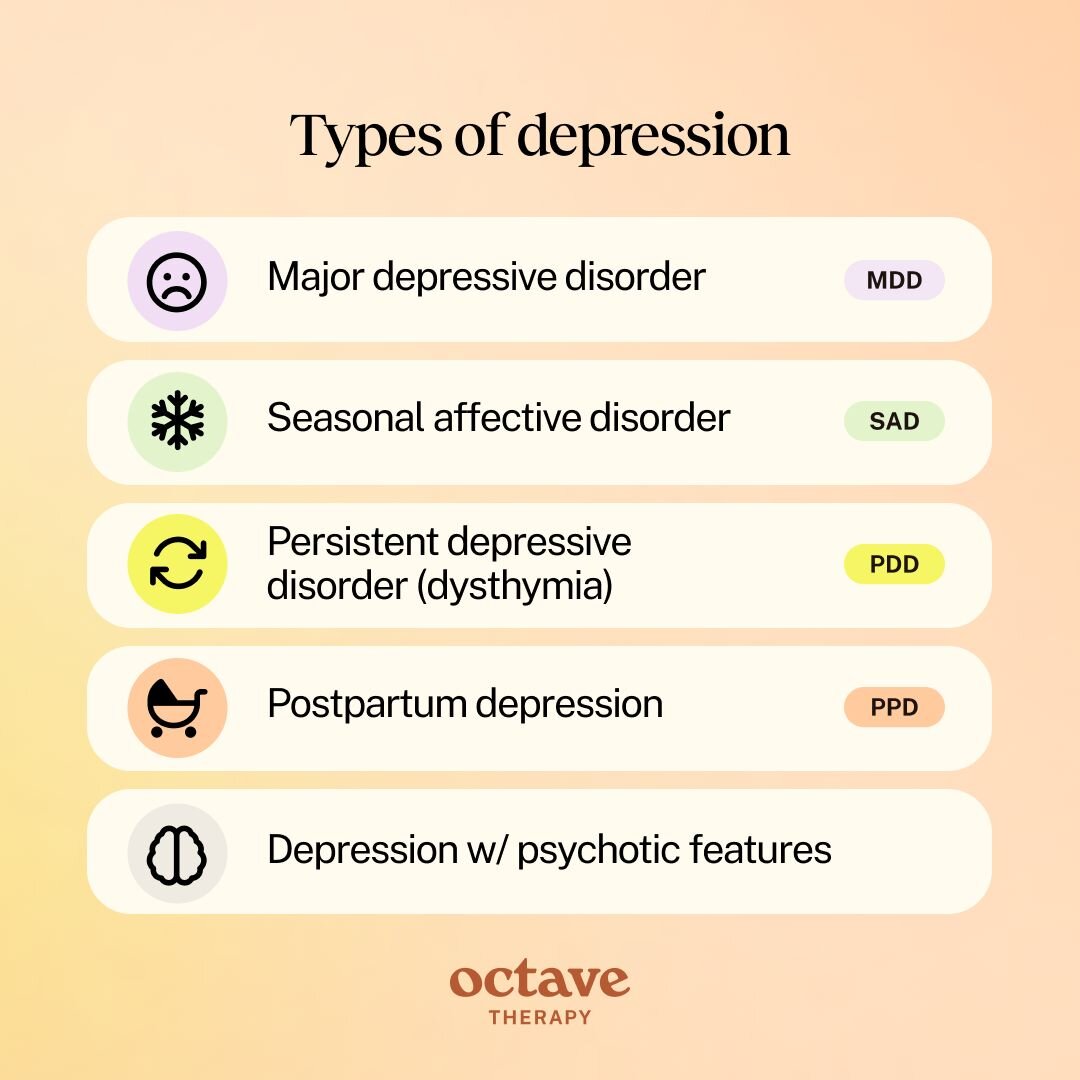
There are a number of different types of depression, each with their own characteristics. Major depressive disorder (MDD) is a clinical diagnosis, characterized by a persistently low mood and/or the less of interest or pleasure in previously enjoyed activities, among other symptoms. A second form of depression is persistent depressive disorder (dysthymia). With this more chronic type of depression, the individual has a depressed mood most of the day for more days than not, lasting at least two years. Postpartum depression and seasonal affective disorder are additional forms of depression that are triggered by specific contexts (the birth of a child or the change of seasons).
Although the term ‘high functioning depression’ has become commonly used in recent years, it is not an official diagnosis. In fact, it is sometimes a description of a person masking depression, keeping up the appearance that they are managing to function as normal.
How To Know if You Are Suffering With Depression
Even when a person is experiencing the most severe symptoms, they may not be aware that they are suffering with depression. Depression can distort a person’s thoughts, feelings, and beliefs, often leading to a deep sense of unworthiness, inadequacy, or even feeling unlovable.
These depression-influenced beliefs can create the illusion that we are not strong enough to handle life’s challenges. However, understanding how depression manipulates our thinking allows us to recognize and challenge these distortions so as to begin the healing process. By rewriting these false beliefs, we can break the cycle that fuels depression and move toward self-compassion and resilience.
How do you know if you are suffering from depression? It’s not as easy as recognizing you are feeling low, but there are still effective ways to identify depression.
You may be suffering with depression if you are:
- Experiencing persistent sadness or a feeling of emptiness
- Consistently feeling irritable, frustrated, or restless
- Feeling guilty and thinking of yourself as worthless
- Experiencing a sense of helplessness and despair
- Unable to feel the interest or pleasure in hobbies or activities you used to enjoy
- Struggling to function in day-to-day life due to these symptoms
If any of these symptoms resonate with you, we encourage you to seek guidance and help. A psychiatrist or therapist can guide you through the process of starting treatment and beginning your journey to recovery.
The severity of depression differs from person to person, as does the impact it has on their ability to function. Furthermore, depression may persist for different lengths of time or only in a specific context. No matter what the case, living with depression can be deeply challenging. But, with support, depression can be managed and one can live with deep fulfillment and meaning.
Let’s get into the types of depression to gain a clearer understanding of what depression is and how it presents.
Types of Depression
Major Depressive Disorder (MDD)
Major depressive disorder (MDD) is characterized by depression that lasts a minimum of two weeks. A major depressive episode causes significant distress and materially impairs functioning. The person might struggle to get out of bed due to the feelings of intense sadness, anxiety, and guilt, while ruminating on harming themselves and/or having thoughts of suicide.
Persistent Depressive Disorder (PDD) or Dysthymia
Persistent depressive disorder (PDD), also known as dysthymia, can be categorized as a less severe form of depression. It lasts for at least two years for adults or one year for children and adolescents and not as many symptoms are required for diagnosis. It is characterized by a depressed mood that lasts for most of the day on more days than not, causing significant distress and impeding functioning.
Depression with Psychotic Features
Depression with psychotic features is a severe subtype of major depressive disorder, characterized by symptoms of hallucinations or delusions during major depressive episodes. Delusions are strong beliefs that contradict evidence to the contrary.
Common delusions are that the person is guilty for causing a disaster, in severe financial straits, suffering from a deadly physical ailment, or that someone is trying to harm them.
Hallucinations refer to hearing, seeing, or feeling things that are not real.
Seasonal Affective Disorder (SAD)
Seasonal affective disorder (SAD) refers to depression that is triggered by a change in seasons. Most commonly experienced in autumn or winter, a person with SAD experiences the onset and alleviation of the symptoms of depression at specific times each year.
Postpartum Depression
Postpartum depression (PPD) is a type of depression suffered by birthing people and/or mothers. Less commonly discussed, but receiving increasing attention and research, is when the other parent or partner of the newborn child experiences postpartum depression. Although it most often occurs in the days or weeks after the birth of a child, it can also start during pregnancy or up to a year after the birth. It is caused by a combination of hormonal changes, psychological factors like low self-esteem, and the stresses of taking care of a newborn baby, and genetics.
Is Depression Common?
Depression is one of the most common mental illnesses, affecting approximately twenty-one million American adults each year. A 2023 Gallup poll found that almost 30% of American adults have been diagnosed with depression during the course of their lifetime. Since not everyone who suffers from depression seeks help, the number of people with depression is likely even higher.
Depression affects youths at an even higher rate than adults. Almost twenty percent of youths aged twelve to seventeen experience depression each year, with rates showing a rapid increase over the past decade.
Statistics suggest that women suffer from depression at a much higher rate than men do (10.3% compared to 6.2% in the U.S.). However, it is likely that depression in males is under diagnosed, with men socialized to express less emotion and exposed to a higher level of stigma regarding depression. Biases in the healthcare system itself may also lead to under diagnosis. Shockingly, the rates of suicide in men are four times higher than in women. This indicates both that many men suffering from depression do not get help and that they are likely to use more lethal means in suicide attempts.
The above statistics specifically relate to the rates of depression in the U.S. Globally, approximately 280 million people in the world suffer from depression each year.
What Are Symptoms of Depression?
That sense that you are navigating life from behind a pair of dark sunglasses is embodied by intense emotions, distorted thoughts, and unhealthy behaviors. The world seems like a different place – one in which the symptoms of depression naturally emerge.
The different types of depression share many of the same symptoms. A person doesn’t need to show all of these symptoms to receive a diagnosis. However, at least one of the following two symptoms need to be present:
- Depressed mood: persistent feelings of sadness, anxiety, or emptiness
- Loss of interest or pleasure
Additional symptoms include:
- Appetite changes: leading to significant weight gain or loss
- Sleep difficulties: struggling to fall asleep, waking up too early, or oversleeping
- Fatigue and lethargy: even after a good night’s sleep
- Physical symptoms: such as aches and pains, headaches, cramps, or digestive problems
- Focus: difficulty concentrating, forgetfulness, or an inability to make decisions
- Troubling thoughts: of death, self-harm, or suicide
- Intense feelings: such as guilt, worthlessness, or helplessness
- Irritability: a sense of frustration, restlessness, or agitation
- Hallucinations or delusions (with psychotic depression)
A diagnosis may be made if a person has experienced five or more of these symptoms, including one of the initial two, over a two-week period or longer.

What Causes Depression?
Depression is caused by a combination of genetics, biological, psychological, and environmental factors. These include the following:
Genetics
Research has consistently shown that a person with a family history is at higher risk of suffering from depression during their lifetime, as well as identifying specific genes associated with the illness. A recent study identified hundreds of additional genes associated with depression by diversifying the sample base.
Brain chemistry
Depression has long been linked to imbalances in the levels of neurotransmitters found in the brain. However, the idea that depression is specifically caused by chemical imbalances is now considered an oversimplification, and the role of neurotransmitters in depression is thought to be far more complex.
Medications that Can Cause Depression
Depression can be triggered by certain medications. Medications for which depression may be a side effect include:
- Anticholinergics: used to treat digestive disorders and respiratory issues.
- Barbiturates: used for seizures and anesthesia. Their sedative effects can suppress activity in the central nervous system.
- Benzodiazepines (benzos): used to treat anxiety and insomnia. Benzos can cause emotional blunting and low motivation.
- Beta-blockers: used for managing heart conditions. Their impact on chemicals can affect mood regulation
- Corticosteroids: anti-inflammatory medications often used for asthma and autoimmune diseases.
- Gabapentin: used for neuropathic pain.
- Isotretinoin: a treatment for severe acne.
- Opioids: used for pain management. With long-term use, opioids can disrupt the production of natural endorphins.
- Proton pump inhibitors: used to treat acid reflux and similar conditions. Their impact on the gut’s microbiome can influence mood.
While these medications can trigger or exacerbate depression, the risk of this side effect is relatively low. We encourage seeking support or guidance if you have concerns about how medication is affecting you. Consulting with your doctor is a valuable way to advocate for yourself, empowering you to feel more in control of your treatment.
Psychology
A person’s psychological health plays a part in causing depression. Many people with depression struggle to regulate emotions and have not developed healthy coping mechanisms. Without healthy management of difficult feelings, their mood dips, especially during a rough patch at home or at work.
Stressful life events
Depression is sometimes triggered by major life changes, trauma, or loss. Even someone with healthy coping mechanisms may struggle to adapt in these circumstances as they are not used to facing such a significant flood of emotions. For a person who already struggles with emotional regulation, stressful life events are particularly difficult to get through.
Medical Conditions
Physical and psychological health are closely connected. People suffering with certain illnesses are at a higher risk of suffering from depression. Chronic health conditions and chronic pain, as well as life-threatening or terminal illnesses, may trigger depression. This is due to both the stress the body is going through as well as the difficult thoughts and feelings that accompany these illnesses.
Substance Use
Alcohol and other substances can trigger or worsen depression. Alcohol is a central nervous system depressant, while other substances can burn through chemicals like serotonin and dopamine, leading to a harsh comedown when the substance wears off. With regular use, the crashes after using substances become worse.
In some instances, this leads the person to repeatedly use the substance so as to get through these lows, leading to a vicious cycle that can become a substance use disorder.
Hormonal factors
Hormonal changes associated with the menstrual cycle, pregnancy, menopause, and other significant life stages can increase the risk of depression in women.
Socioeconomic circumstances
People living in difficult socioeconomic circumstances are at higher risk of depression. They may have bigger responsibilities, face greater challenges, and have less time for self-care. Socioeconomic factors also play a major role in how much access a person has to mental healthcare services.
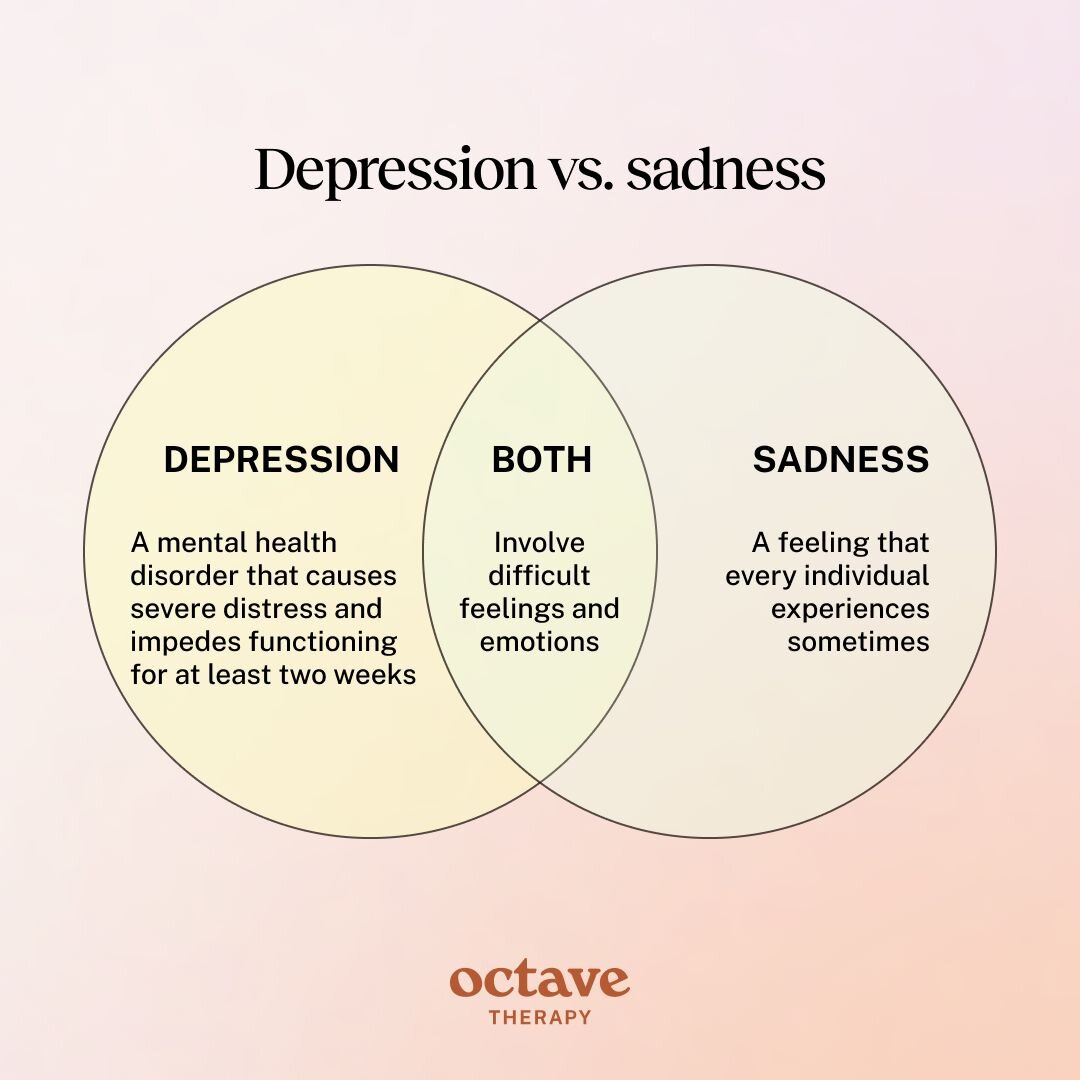
What is the Difference Between Depression & Sadness?
Depression and sadness are used interchangeably by many people, but the words refer to very different experiences. Sadness is a feeling that every individual experiences sometimes. It can be painful and difficult to process, but it is a healthy manifestation of disappointment, loss, and other normal aspects of life.
Depression, on the other hand, is a mental health disorder that causes severe distress and impedes functioning. Sadness presents as one of the symptoms of depression, along with feelings of emptiness, guilt, and worthlessness. The person with depression struggles to regulate these emotions, leading them to increase in intensity and become a major source of distress.
Depression Diagnosis
A person experiencing the symptoms of depression should seek a diagnosis from a mental health professional. All licensed therapists are qualified to make a diagnosis. Getting a diagnosis is important for the following reasons:
- It provides you and your therapist with clarity on the kind of help you need. They can then work with you and other mental health professionals on a collaborative treatment plan.
- The diagnosis is provided to your health insurance provider to ensure they pay for the treatment you require.
At Octave, we provide diagnosis for both of these purposes. Your therapist will guide you through the process to determine a diagnosis, as well as the next steps in comprehensively treating depression.
When additional mental healthcare services are necessary, Octave will provide you with resources and referrals to make the process as seamless as possible.
How is Depression Diagnosed?
During an assessment for depression, your mental healthcare provider will begin with an interview, asking you about your mental and emotional state, as well as any behavioral changes you have noticed. They will also ask about any family history of mental illness. Since depression has a genetic component, people with family members with depression are more likely to suffer from the disorder.
During this interview, they begin to get clarity on why you think you might be suffering from depression. They also get a better idea of some of the areas which they need to explore further. In many cases, they will have a fairly good sense of whether you have depression, but it is still necessary for them to consider all possibilities.
In order to get a more comprehensive outline of your symptoms, therapists at Octave will use the Patient Health Questionnaire-9 (PHQ-9) to provide a baseline at the start of your treatment and, later, to assess its effectiveness.
Your provider will test for other mental health conditions which may be responsible for the symptoms of depression. This may lead to an alternative diagnosis. Alternatively, they may diagnose two or more co-occurring disorders. Common disorders that co-occur with depression include anxiety disorders, eating disorders, and substance use disorders.
Criteria for a depression diagnosis
The DSM-5 sets out the criteria necessary for a depression diagnosis. A person must have experienced at least five of the symptoms of depression. At least one symptom must be a depressed mood or loss of interest in pleasurable activities (anhedonia).
These symptoms need to have persisted for a period of two weeks or longer, during which they are present on most days for most of the day. In the case of persistent depressive disorder (PDD) or dysthymia, they need to have been present for at least one year for adolescents and two years for adults.
Management and Treatment of Depression
An official diagnosis from a healthcare or mental health provider is the first step towards healing. Once you have received your diagnosis, they will collaborate with you on identifying your goals in order to recommend the most appropriate course of treatment. Treatment generally involves medication, therapy, or a combination of the two.
Medication for Depression
Antidepressant medication works by increasing the levels of neurotransmitters associated with depression. Over decades of refinement, their efficacy has improved significantly while side effects have become less common and less severe.
Common antidepressant medications include:
- Selective serotonin reuptake inhibitors (SSRIs): By inhibiting its reuptake, SSRIs increase the levels of serotonin in the brain. Common SSRIs include fluoxetine, sertraline, and citalopram.
- Serotonin-norepinephrine reuptake inhibitors (SNRIs): SNRIs inhibit the reuptake of norepinephrine in addition to serotonin and can be effective for people who do not respond to SSRIs. Common SNRIs include venlafaxine and duloxetine.
- Atypical antidepressants: Certain antidepressants work by increasing the levels of other neurotransmitters, such as dopamine. A common example is bupropion (Wellbutrin, among other brand names).
- Tricyclic antidepressants: These antidepressants work by inhibiting the reuptake of serotonin and/or norepinephrine. However, they are among the earlier classes of antidepressants and, as such, they can cause more side effects and are only used when other antidepressants have not worked.
Emerging Medications for Depression
In recent years, ketamine and its derivative esketamine have emerged as effective alternatives for treatment-resistant depression. By increasing levels of glutamate, the brain’s most abundant chemical messenger, esketamine impacts more brain cells at once.
Esketamine is a hugely promising treatment. Unlike traditional antidepressants which can take two weeks or longer to have an effect, esketamine works rapidly, providing relief in just a matter of hours. It is administered through a nasal spray and its side effects are short-lived, peaking after about forty minutes before wearing off.
However, since use of esketamine for treating depression is fairly new, it has been approved specifically for people who haven’t responded to other treatments and is administered in a clinical setting. With further research, esketamine has tremendous potential to become a first-line treatment.
Therapy for Depression
Therapy is an effective treatment for depression, often used independently or in conjunction with medication. There are multiple different kinds of therapies for treating depression. Most therapists use one or a combination of the following therapies:
- Cognitive behavioral therapy (CBT): The most widely used type of therapy, CBT works by identifying and challenging thought and behavioral patterns that contribute to depression. In the decades since its development, CBT has become extremely popular due to its effectiveness as a time-limited or short-term therapy.
- Dialectical Behavior Therapy (DBT): DBT has gained prominence in recent years as an effective treatment for depression. Rooted in Eastern mindfulness principles, it trains the person in practical skills for regulating emotions, increasing their capacity to cope with emotional overwhelm and high levels of distress.
- Psychodynamic therapy: Through an exploration of the person’s unconscious thought processes and past experiences, psychodynamic therapy is effective at resolving inner conflicts that contribute to depression. While it is a more long-term approach than CBT, many people find it useful in their search for individuality and purpose, contributing to its enduring appeal.
- Interpersonal therapy (ITP): Often used in conjunction with CBT, ITP seeks to improve problematic relationships and circumstances contributing to the person’s depression.
What Should I Expect Living With Depression?
Living with untreated depression causes a person severe distress, making it difficult to function or even get out of bed. Coping mechanisms that once worked no longer seem effective and enjoyable activities lose their appeal.
There are also other issues that depression can cause if left untreated. These include:
- Health problems: People with untreated depression are at higher risk of cardiovascular issues such as heart attacks, heart failure, and arrhythmia. The brain is at risk of unhealthy structural changes that can lead to cognitive impairment. There is also a link between untreated depression and diabetes.
- Anxiety: With a persistent sense of ‘wrongness’, the person may become more anxious, catastrophising even the most innocuous situations.
- Risky behaviors: Since their usual coping mechanisms are not working, the person might engage in risky behaviors as an attempt to get a ‘rush’ or even to harm themselves.
- Substance abuse: As an attempt to distract from or drown out the difficult thoughts and feelings, the person may turn to substances. The effect is fleeting and, after the comedown leaves the person feeling worse than before, they use more substances, leading to a vicious cycle.
- Relationship problems: Depression makes it difficult to interact with others as normal. Relationships deteriorate as the person withdraws and their partner begins to feel abandoned.
- Suicide: At its most extreme, depression can be fatal. The person has suicidal thoughts, believing things will not get better and questioning if life is worth living.
How to Live With Depression
It is essential to get treated for depression as soon as possible. Nonetheless, if you do not have access to mental healthcare services or are on a waiting list, there are steps you can take to live with depression in the meantime.
Try to maintain the following behaviors:
- Practice self-care: Low motivation and a low sense of worth can make it difficult to practice self-care. However, it is now more important than ever. Take time to do soothing activities and treat yourself when possible. Look for things which do not take too much energy and which will benefit your wellbeing, even if they do not provide pleasure right now.
- Connect with others: The tendency to isolate when living with depression is common. Unfortunately, isolation only exacerbates the symptoms. Confiding in your loved ones when you are struggling may help lighten the load. You may feel less alone and a stronger sense of security.
- Maintain health and hygiene: If you're struggling to get out of bed, showering, brushing your teeth, and sticking to a healthy routine can seem overwhelming. Since poor physical health exacerbates depression, determine what’s realistic for you to do each day, even if it is just taking a shower or keeping up with prescribed medication or supplements.
- Be patient with yourself: People with depression tend to judge themselves for their illness. However, self-worth is important. Remind yourself that you are not to blame for your health condition. You will get better, even if it takes a bit of time.
When to Seek Help for Depression
A common question people ask themselves is ‘how do I know if my depression is bad enough to get help?’ If this sounds familiar, it is time to get help.
The lingering misconception that depression is a weakness leads many individuals to put off seeking treatment, believing they should ‘get over it’ themselves. But waiting until things get worse only leads to more suffering.
If you are experiencing one or more of the symptoms of depression, get in touch with a mental health professional immediately. They will help you determine if you are suffering from depression and provide a treatment plan.