What is Post Traumatic Stress Disorder (PTSD)?
Overview
Living with post-traumatic stress disorder (PTSD) can feel like being in two places at once. It gives one the sense that the present reality is never quite as safe as it seems. The person affected has lived through a trauma and, although months or even years have passed, they still feel like they're in the same situation.
This experience is not merely a consequence of taking extra care in the wake of a tragedy. Rather, it arises from the dysfunction of physical and psychological stress responses. During a traumatic event, a person’s body and mind activate survival mechanisms to help them respond appropriately in the moment. PTSD occurs when those mechanisms continue to operate long after the trauma has ended. In effect, the person remains switched ‘on’ as if their life is at risk.
Not all people who go through a trauma experience PTSD and not all trauma-related stress is indicative of a disorder. It is normal for stress symptoms to remain in the days or weeks after a trauma. PTSD is only diagnosed when the symptoms are present more than a month later and are impeding the person’s day-to-day functioning.
In this guide, we will explore what PTSD is, its signs and symptoms, causes, treatment, and how you can help someone suffering from PTSD. We will discuss the differences between normal trauma-related stress and PTSD, as well as the nuances of complex PTSD (CPTSD), a common subtype of the disorder receiving increasing recognition.
What is Post-Traumatic Stress Disorder (PTSD)?
Post-traumatic stress disorder (PTSD) is a mental health condition that a person can develop after experiencing a traumatic event. With PTSD, the body and mind remain in a stress response as if the threat is still present, months or years after the trauma occurred. Approximately 3.6% of American adults develop PTSD each year.
PTSD was once thought of as a condition faced by military veterans after coming back from war. At various times, it was called ‘shell-shock’ and ‘combat fatigue’ and not treated as a mental illness. In fact, a stigma surrounded it, with veterans who developed the condition considered ‘weak’ and expected to just get over it.
Today, however, we understand that any individual can develop PTSD after a trauma. It has nothing to do with strength or bravery but rather with the natural human response to a threat. That stress response is a function of a person’s survival instinct, without which they would not react appropriately in order to protect themselves.
Since the stress response is activated by a threat in any form, it is common among people who survive all forms of trauma, including physical and sexual assault, accidents, and bullying. It can also develop in a person who has suffered a sudden loss or whose loved one has experienced a trauma, even if the person was not present when it happened. Furthermore, emergency and first responders can also be diagnosed with PTSD after “experiencing repeated or extreme exposure to aversive details of the traumatic event(s).”
Symptoms of Post Traumatic Stress Disorder or PTSD
Recognizing the signs of PTSD is not as simple as assessing one’s mood in the wake of a traumatic event. Trauma affects everyone, whether or not they suffer from PTSD. It can trigger intense emotions, shake up a person’s perception of the world, and lead to lifelong consequences, including the possibility of being retraumatized when experiencing a similar event.
As such, while PTSD often presents with symptoms like numbness, anxiety, negative beliefs about oneself, and loss of interest in previously pleasurable activities, these may instead point to a diagnosis of depression, anxiety, or other mood disorders.
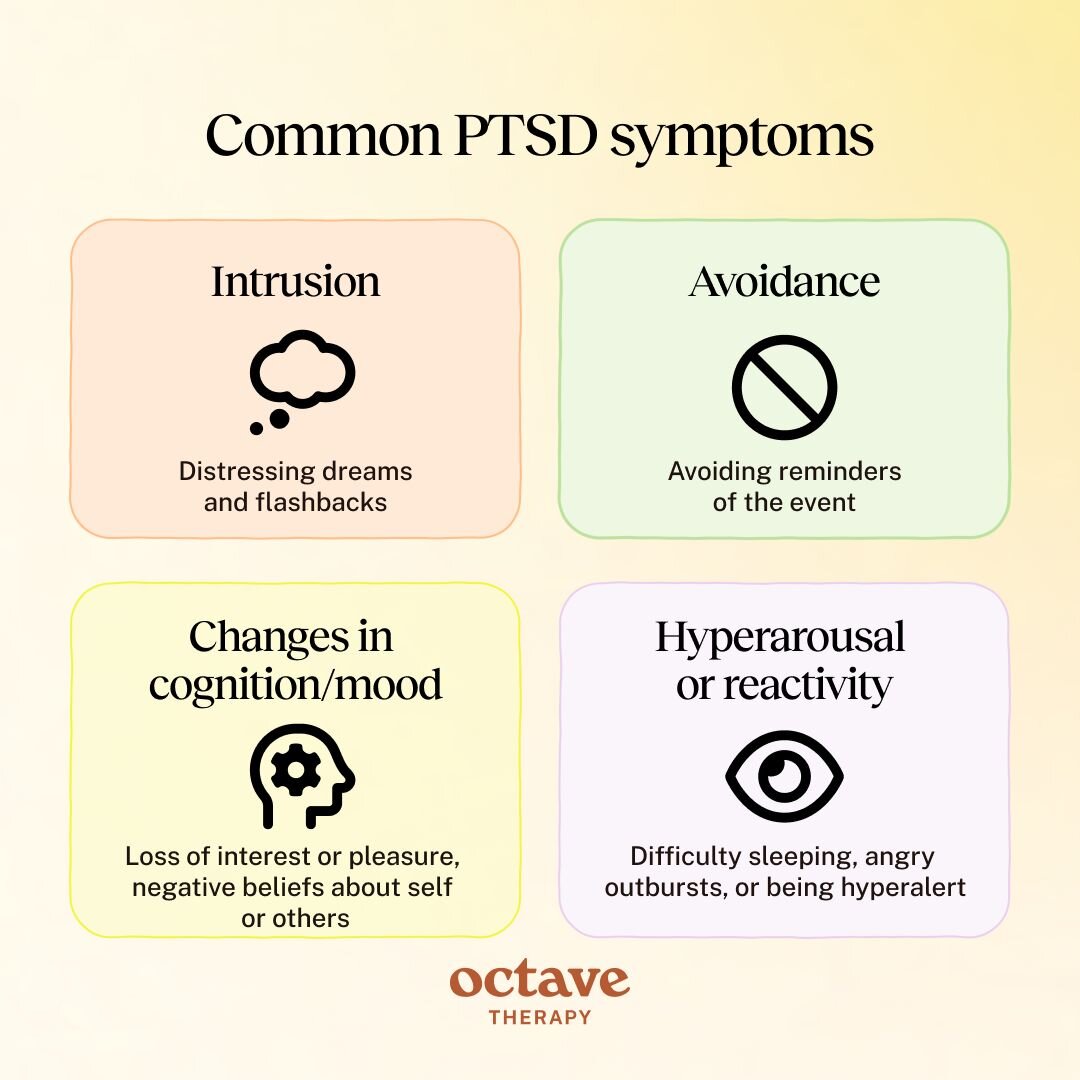
The symptoms of PTSD are separated into four categories. One or more symptoms of each category need to be present for a PTSD diagnosis. They include:
- Intrusion: Cognitive symptoms include repeated, involuntary memories; distressing dreams; or flashbacks of the traumatic event. Physical symptoms include racing heart; nausea, sweating.
- Avoidance: Trying not to think about the event; avoiding potential reminders such as places, people, situations, and objects associated with it.
- Changes in cognition and mood: Struggling to remember details of the event; thinking negatively about oneself and others; feelings of fear, anger, horror, guilt, and shame; loss of interest or pleasure; blaming oneself or others; a sense of detachment.
- Hyperarousal or reactivity: Being hyperalert and overly watchful; paranoid thoughts; irritability; being quick to anger; difficulty sleeping; being easily startled.
The combination of symptoms leads to changes in behavior and lifestyle, as the person adjusts to compensate for or avoid the symptoms. They withdraw from social situations and search for new coping mechanisms, often leading to the use of substances which numb feelings and cloud thoughts.
What is the Difference Between Stress vs PTSD?
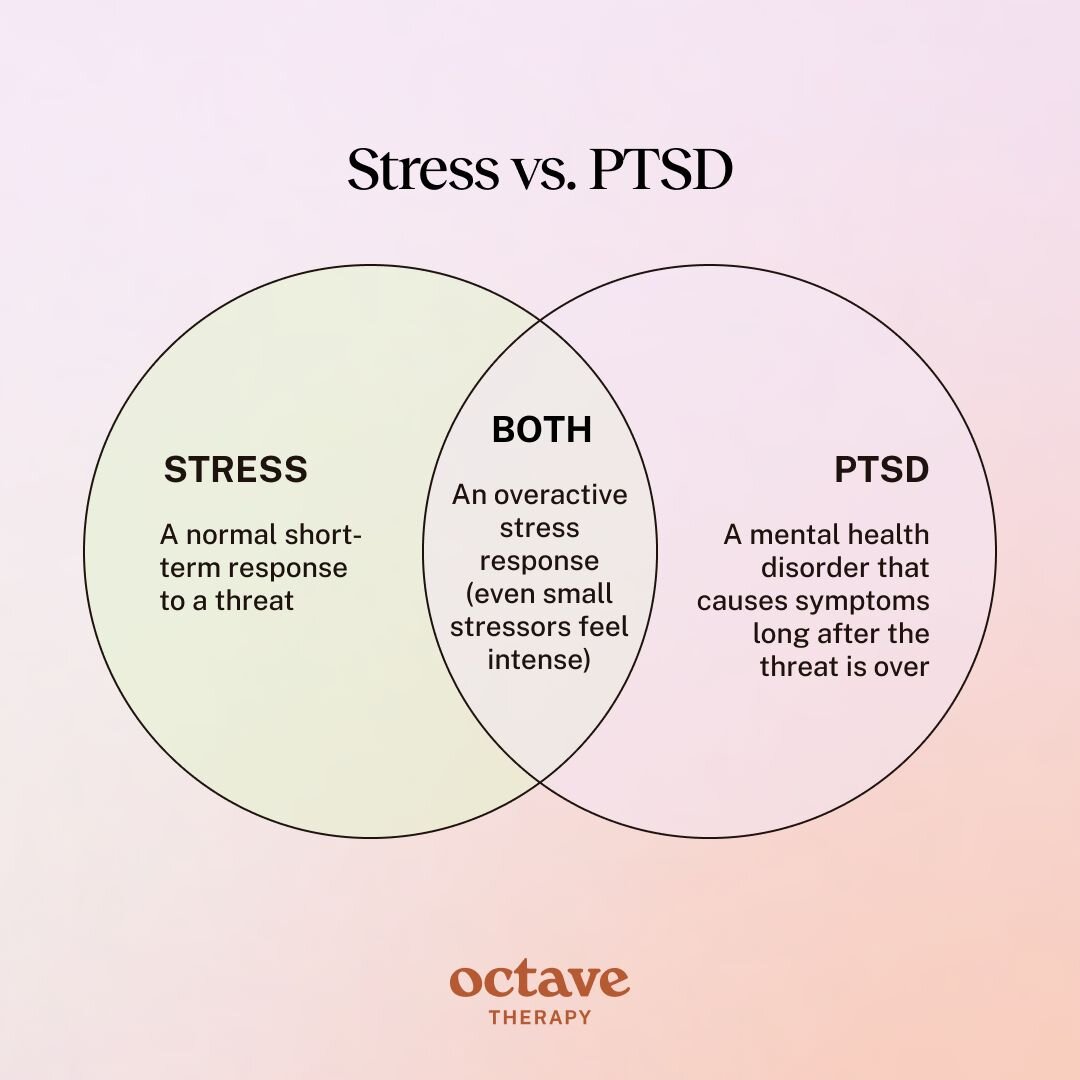
Everyone experiences stress throughout their lives. After a traumatic event, stress often becomes more intense and frequent or consistent. What is the difference between stress and PTSD?
Stress is the body’s natural response to difficult situations and threats. The nervous system is activated so as to prepare the person to use strategies such as fight or flight. In the face of danger, common stress responses include fear, hyperawareness, the release of adrenaline, and a racing heart.
Stress is a necessary component of human experience and is often helpful. It is when the stress response is overactive that it can become harmful.
After a trauma, many people experience acute stress disorder (ASD). This comes about shortly after the event and may present with similar symptoms to PTSD. However, ASD is experienced for a limited period of three days to a month.
The main difference between PTSD and ASD is that PTSD symptoms persist for longer than a month. They can continue for months or years after the event and usually require treatment in order to subside.
In addition, although symptoms of PTSD and ASD can both appear shortly after the event, PTSD symptoms may only show up months or, in some cases, even years later. Some symptoms, such as anger, may not even be recognized as trauma responses until they become persistent and problematic.
Stress
Definition: A healthy short-term response to a threat, with the body and mind activating survival mechanisms.
Duration: During the event and potentially days or weeks after its completion. Resolves on its own.
Physical Symptoms: Racing heart, sweating, headache, tension.
Emotional Symptoms: Anxiety, fear, sadness, and agitation at an intense level.
Thoughts & Behaviors: Thoughts temporarily racing or mind blanking. Fight-or-flight (or freeze or fawn) behaviors.
PTSD
Definition: A mental health disorder that can develop after experiencing a traumatic event, with stress responses remaining active long after the threat is over.
Duration: Persisting for at least one month after the traumatic event. Often lasts months or years and requires professional treatment.
Physical Symptoms: Hypervigilance, hyperreactivity, insomnia, flashbacks, nightmares.
Emotional Symptoms: Persistent and intense feelings of fear, anxiety, shame, guilt, numbness, depression.
Thoughts & Behaviors: Negative thoughts about oneself, others, or the world. Dissociation. Avoidance of trauma-related memories, places, people, and items. Self-destructive behaviors.
What is Complex PTSD?
PTSD became an officially recognized diagnosis in 1980, helping millions of people make sense of what they were going through or had been through. Its presence in diagnostic manuals also made it easier to identify when someone was struggling with PTSD and to get them help. However, there were still many cases of mental illness related to trauma that did not fit the common understanding of PTSD and its treatment.
In particular, people who had been through extended periods of physical or mental suffering in their lives showed many symptoms of PTSD, even when there was no specific instance that fit the traditional definition of a traumatic event. Similarly, people who during such a period experienced traumatic events on repeated occasions presented differently to those with typical PTSD. Recently, there has been increasing recognition that this can include people who have been in emotionally abusive relationships.
Cases like these have become known as complex PTSD. Complex PTSD (CPTSD) develops after experiencing repeated or prolonged trauma, often during childhood.
A person who grew up in a household with consistent parental neglect may develop CPTSD, having spent years navigating life without a sense of internal or external safety. Whether or not they went through a typical traumatic event, their body’s stress response needed to be constantly active during a time which could be considered a prolonged trauma. They have CPTSD if their stress response remains active even when they transition to adulthood or are taken into a secure home and family.
In another instance, a person may live in a household with an abusive parent or partner. They suffer abuse frequently – perhaps even daily. These instances of abuse fit the traditional definition of trauma and even one such occasion can lead to PTSD. However, the repeated experience of the trauma engenders characteristics different to traditional PTSD.
People who suffer from CPTSD often face the following challenges in addition to typical PTSD symptoms:
- Difficulty regulating emotions: Due to the consistent presence of trauma in a period of their lives, the person begins to struggle to regulate their emotions appropriately. The sense of danger may have necessitated intense emotional responses which cause significant distress when their situation has changed.
- Distorted self-perception: A person who has faced an extended period of neglect, abuse, or mistreatment may start to see themselves in distorted ways, leading to struggles with shame and guilt, a sense of worthlessness, and the belief that something is wrong with them.
- Interpersonal struggles: Emotional dysregulation and distorted self-perceptions impact how a person interacts with others, but it is the difficulty trusting others that can make interpersonal relationships particularly volatile for people with CPTSD.
What Causes PTSD?
As part of our natural survival instinct, the human body and mind evolved defense mechanisms that kick in when faced with a threat. This phenomenon is often referred to as the fight-or-flight response, referring to the two most common reactions. More recently, research has recognized other mechanisms like ‘freeze’ or ‘fawn’.
A Healthy Threat Response
A person’s survival mechanism is expressed both in their physical reactions and their emotional responses once the brain detects a threat. The amygdala, the part of the brain responsible for detecting threats, sends a signal to the hypothalamus, the ‘control center’ for bodily functions. The hypothalamus, in turn, activates the autonomic nervous system (ANS).
In particular, it triggers the part of the ANS known as the sympathetic nervous system (SNS), which is responsible for the automatic processes of fight-or-flight. This leads to the physiological responses intended to prepare the person to protect themselves, such as a racing heart, the release of adrenaline and cortisol, increased oxygen flow, and dilated pupils.
While the threat is active, these responses help a person survive by providing more energy, awareness, and reactivity, among other things. When the danger is no longer present, the ANS returns to its normal functioning, ready to deal with the experiences of everyday life.
The Stress Response and PTSD
PTSD develops when the person’s stress response does not return to normal. The SNS remains overactive as if the traumatic event is still happening. The body and mind continue to react in ways which can be helpful when a person is in danger but which are otherwise maladaptive.
People with PTSD therefore remain hyperaware and overreactive, with many symptoms of PTSD resembling stress responses. Over an extended period of time, these responses can affect the way the person thinks about themselves and the world, impacting day-to-day life and interpersonal relationships.
Events That Lead to PTSD
PTSD develops after a person experiences a traumatic event. While the type of event can differ for each individual, common causes of PTSD include:
- Military combat: including experiencing threat in battles or ambushes, as well as seeing or committing violent acts which go against their value systems.
- Sexual assault: with the risk especially high when the perpetrator is known.
- Physical assault: including domestic violence and violent crime.
- Accidents: car and airplane crashes, industrial accidents, or even falls which lead to severe injury.
- Natural disasters: often involving loss of loved ones, destruction of homes, or displacement.
- Medical trauma: especially when long-term or permanent injury is involved, or when an illness is life-threatening or terminal.
- Bullying: which is often repeated, physically or verbally abusive, and personal.
- Repeated exposure to traumatic events: such as first responders who frequently see and hear details of trauma events.
Survivors of war – and especially refugees – are at high risk of PTSD, having endured extended periods of instability, mass violence, persecution, and captivity.
PTSD can develop even when the person was not physically involved or present in the traumatic event. Examples include:
- The death of a loved one, especially when sudden.
- Learning a loved one went through a trauma.
- First responders frequently present at accident sites.
- Medical workers experiencing the death of patients.
How To Help Someone with PTSD
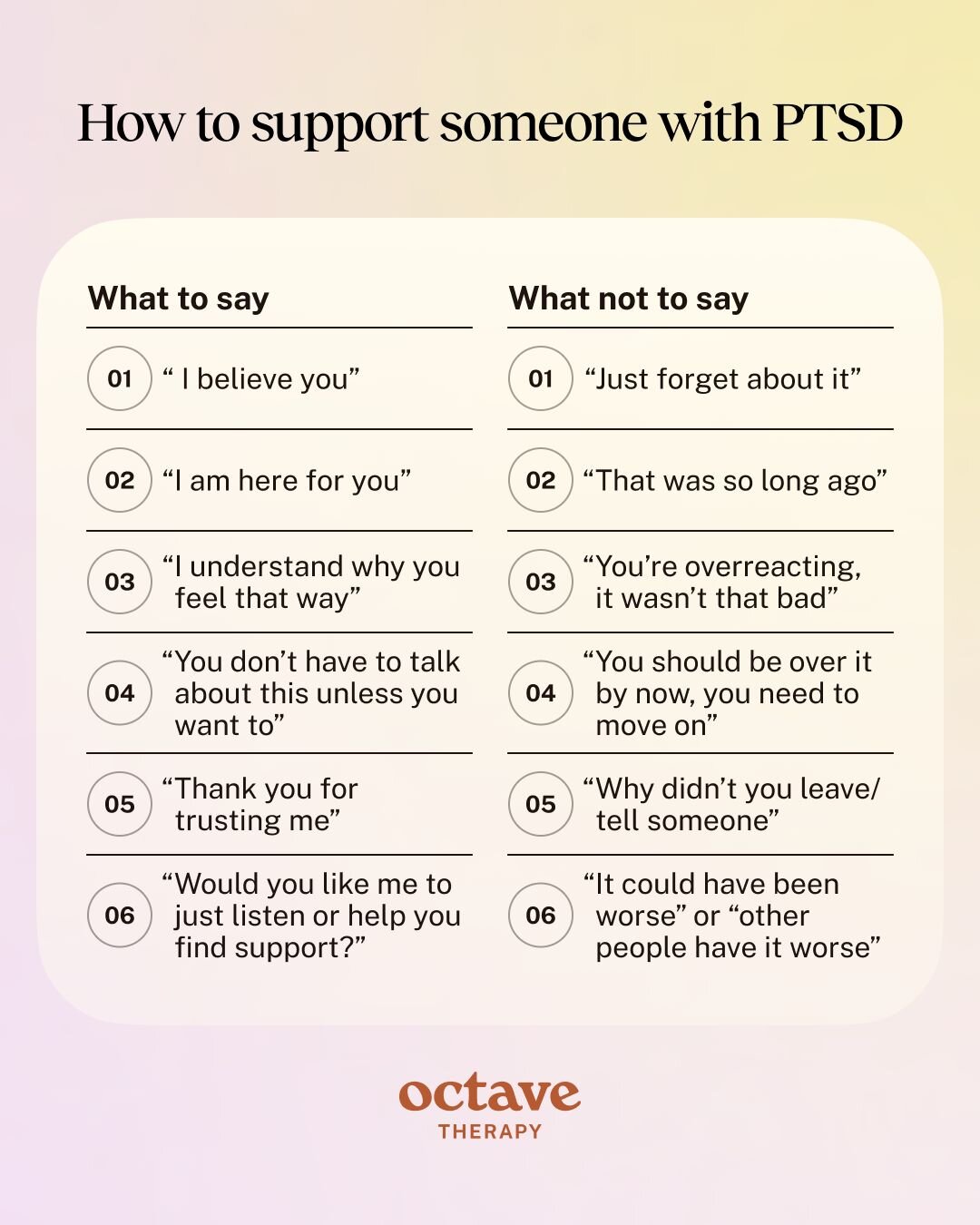
If you have a loved one suffering with PTSD, you might be feeling helpless. You have tried to give them the support they need but nothing you do seems to make a difference. You feel lost and guilty. Shouldn’t you know how to help them?
It is normal to feel this way but the reality is that you cannot magically heal them, no matter how hard you try. PTSD is a mental health condition that requires professional treatment. Although you can encourage them to get treatment and help with the admin, you can’t make decisions for them. Neither can you control how soon they are able to access treatment or its effectiveness.
Nonetheless, there are some things you can do in the meantime to provide some relief and help them feel less alone.
Listen
It’s natural to want to actively help your loved one when they tell you about their pain. However, advice is not what they need right now. When you simply listen to them, however, you show them that they’re not alone. Their pain won’t disappear, but talking to you might lighten their burden.
Validate Their Feelings
When a person with PTSD tells you about feelings of fear, shame, and guilt, you may be tempted to respond by explaining why they don’t need to feel the way they do. Unfortunately, no matter how logical your explanation may seem, the feelings will remain. Your loved one may feel unheard or even ashamed for feeling this way, leaving them reluctant to broach the subject again.
Instead, validate their feelings with empathy. Empathy is about understanding where another person is coming from, even if it differs from your context. When you put yourself in their shoes, you get a clearer picture of how they feel without having to take their feelings on yourself.
Respect Their Boundaries
It’s possible that you carry your concern for your loved one with you throughout the day. This may lead you to constantly check in on them or try to get them to make healthier decisions. However, PTSD often leads to a feeling of overwhelm, resulting in feelings of frustration with themselves and others, as well as difficulties with anger management. They may need space and may not have the capacity to do certain things, even when they know they’d feel better if they did.
Ask them what they need and respect their boundaries, while using your discretion if you see them engaging in dangerous behaviors.
Encourage Professional Help
Many people who suffer from PTSD do not seek professional help at first, believing that they should ‘just get over it’. In some places and communities, there is still a stigma surrounding mental health and people are reluctant to get treatment. Sometimes, a person simply does not believe that they can be helped.
You can’t force your loved one to get professional help but you can explain what it is and why it’s necessary. Encourage them with gentleness and, if you start feeling upset at their refusal, take a break rather than expressing your frustration. Pushing them to get help can trigger a defensive response, making them less likely to agree.
Educate Yourself on PTSD
Knowledge is power, as they say, and in this case it will help you make the best decisions when relating to your loved one. Educating yourself on PTSD ensures you get perspective on what they’re going through and clarity of what they need.
Be Patient
Recovering from PTSD takes time, even when the person is getting treatment. Be patient with your loved one, continuing to help in the ways you can. Remember to also take care of your own wellbeing – running on empty does yourself and your loved one a disservice.
Treatment for Post-Traumatic Stress Disorder (PTSD)
Therapy is the primary treatment for PTSD. It focuses on helping the person process the trauma and reduce symptoms, leading to better wellbeing and functioning in daily life.
The therapies most commonly used to treat PTSD include:
- Cognitive-Behavioral Therapy (CBT): CBT challenges the thoughts and perceptions associated with PTSD, systematically using logic to change or reframe them. The difficult thoughts and feelings gradually lose their power. The therapist trains the person to use CBT skills outside of therapy as well, helping them restructure maladaptive thought processes.
- Prolonged Exposure Therapy (PE): PE is a type of CBT which focuses on slowly exposing the person to elements associated with the trauma in a safe environment. It usually begins with some of the less triggering thoughts and memories. As the person’s resilience improves, they face more distressing memories and triggers.
- Cognitive Processing Therapy (CPT): Another type of cognitive-behavioral therapy specifically designed to treat Post-traumatic Stress Disorder (PTSD). It involves identifying and challenging unhelpful thoughts and beliefs related to the traumatic experiences, ultimately leading to a more balanced and accurate understanding of the event.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR is a method of therapy that involves moving your eyes and tapping while recalling traumatic events. This helps the person reprocess these memories, reducing their vividness and the emotions associated with them. Research has shown that EMDR is highly effective and it is considered one of the frontline treatments for PTSD.
- Internal Family Systems (IFS): IFS therapy conceptualizes the mind as a system of interconnected “parts” and is seen as a valuable approach for trauma. It works by helping the person identify and heal the parts of their mind that are wounded and protective, leading to increased self-compassion and resilience.
Medications for PTSD
There are no specific PTSD medications. However, certain psychiatric medications are used in conjunction with therapy to treat the symptoms of PTSD.
- SSRIs and SNRIs: These common antidepressants help regulate mood, anxiety, and intrusive thoughts.
- Prazosin: An antihypertensive, used to treat high blood pressure, prazosin has shown effectiveness at reducing nightmares associated with PTSD.
- Antipsychotics: Atypical antipsychotics, including risperidone and quetiapine, may be used in cases of severe or treatment-resistant PTSD. Due to their high side effects, they are prescribed only if SSRIs and SNRIs are unhelpful.
When to Seek Help for PTSD
If you have experienced a traumatic event or long-term trauma and are suffering from symptoms of PTSD, we encourage you to seek help as soon as possible. PTSD is a mental health condition that requires treatment. The sooner you get professional help, the sooner your recovery from PTSD begins.
Start by making an appointment with a therapist. A therapist will help determine if you are suffering from PTSD and will work with you to create a treatment plan.