What is Obsessive Compulsive Disorder (OCD)?
Overview
Do you have recurring, anxiety-provoking thoughts that you cannot control? Are you compelled to carry out specific actions, certain that something will go terribly wrong if you don’t? You may be suffering from obsessive-compulsive disorder (OCD).
Distressing thoughts can feel overwhelming. Anyone who has ever suddenly questioned whether they left the stove on can empathize with how easy it can be to picture every worst-case scenario. This thought can drive the person to rush home to check, even if they’re fairly sure they turned the stove off.
With OCD, a person is beset by distressing thoughts that may encompass a range of scenarios. These thoughts are powerful and persistent and may occur on a daily basis. They are accompanied by the compulsion to perform actions that quell the thoughts temporarily.
Unlike the common scenario with the stove, the obsessive thoughts of OCD are often not rational, fixating on scenarios that are highly unlikely or even impossible. The compulsions do not necessarily relate to the thoughts, either, and more closely resemble rituals, many of which have no logical basis.
OCD is regularly misrepresented, which has led to the term being casually thrown about to describe a mere preference for cleanliness or order. As such, it is important to understand the ins and outs of the disorder so that you can recognize it and know when to seek treatment.
This guide will cover what OCD is, some common subtypes of OCD, and the symptoms of OCD, as well as its various treatments.
What is Obsessive-Compulsive Disorder (OCD)?
Obsessive-compulsive disorder (OCD) is a mental health condition characterized by obsessive thoughts, followed by the compulsive performance of actions to alleviate the anxiety caused by the thoughts. The actions provide only temporary relief, however, leading to a cycle that is disruptive to the person’s life.
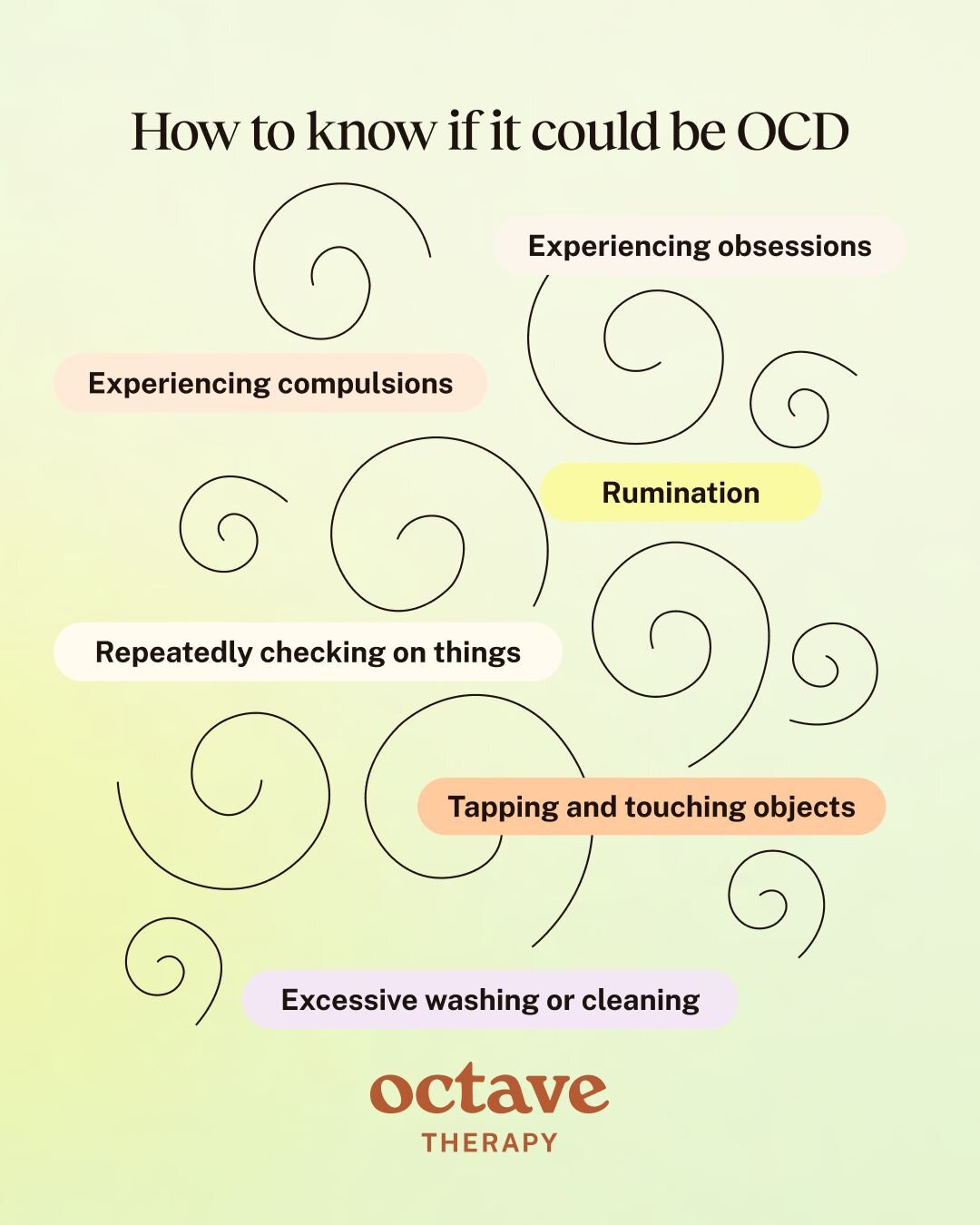
How to Know if You Are Suffering With OCD
Obsessive thoughts are not necessarily a sign of OCD. On occasion, everyone has recurring thoughts that can be distressing. Someone getting married might frequently think about potential issues that may arise, such as whether estranged family members will turn up. A person who has a loved one suffering with an illness may repeatedly think about the person’s suffering or their potential loss. People who struggle with anxiety disorders also sometimes have obsessive thoughts about worst-case scenarios.
How do you know if you are suffering with OCD or just having general obsessive thoughts? The following are typical experiences for people with OCD.
Experiencing Obsessions and Compulsions
Obsessions are more persistent and intrusive than general intrusive thoughts or worries. When an obsession is a symptom of OCD, it tends not to dissipate on its own. In addition, it is difficult to turn your attention to anything else while it is present.
Furthermore, obsessions that are symptoms of OCD often, though not always, lead to compulsions. Compulsions are not the same as the urge to act in a practical way to solve a problem. Rather, they are ritualistic acts to provide temporary relief from the obsession itself.
Checking on Things Repeatedly
Repeatedly checking on things is a common compulsion for people with OCD. This kind of compulsion may seem similar to how anyone might respond to an obsessive thought. For example, a person with OCD who worries they left the stove on might feel compelled to check whether they in fact did so. However, this compulsion will often be subject to “rules,” such as checking the stove a specific number of times or touching the knobs a certain way.
These repeated checks are not carried out due to forgetfulness or realistic concerns, but rather as a result of the intense anxiety and doubt caused by the obsession. The person will perform these checks even when they know that there is no real reason to do so.
Certain kinds of checking are common for people with OCD. They include:
- Safety: checking that doors and windows are locked, stoves and heaters are turned off, faucets are closed, etc.
- Health: checking for moles or lumps, irregularities with breathing or heartbeat, temperature, etc.
- Hygiene: checking for stains on clothing, body odor, bad breath, etc.
- Work or academic: checking for errors in work or schedules, that documents are not lost, etc.
- Relationships: asking for reassurance, checking for signs of infidelity, etc.
- Religion or morality: checking that rituals or prayers have been carried out correctly, that no rules have been broken, etc.
Excessive Washing or Cleaning
People with certain types of OCD, especially contamination OCD, compulsively wash their hands, faces, or bodies, and/or repeatedly clean their homes, possessions, or clothes. This is not equivalent to a preference for neatness or cleanliness. The excessive nature of compulsive washing or cleaning disrupts daily life and can even cause harm, such as dermatological problems.
Rumination
Rumination is a common characteristic of OCD. Unlike obsessive thoughts, which are intrusive and cause immediate distress, rumination refers to overthinking driven by anxiety about certain questions or themes. It is itself a compulsion that the person engages in as an attempt to relieve their anxiety.
Tapping and Touching Objects
Tapping and touching specific objects are common compulsions for people with OCD, often driven by magical thinking in regards to an obsession. For example, a person may feel compelled to tap an object a certain number of times to ward off a catastrophe. In other cases, they may feel the need to create symmetry or balance through actions such as touching the object with both hands or stepping on a crack with both feet. Some people touch and tap objects in an attempt to achieve a particular sensory experience, driven to do so until it “feels right.”
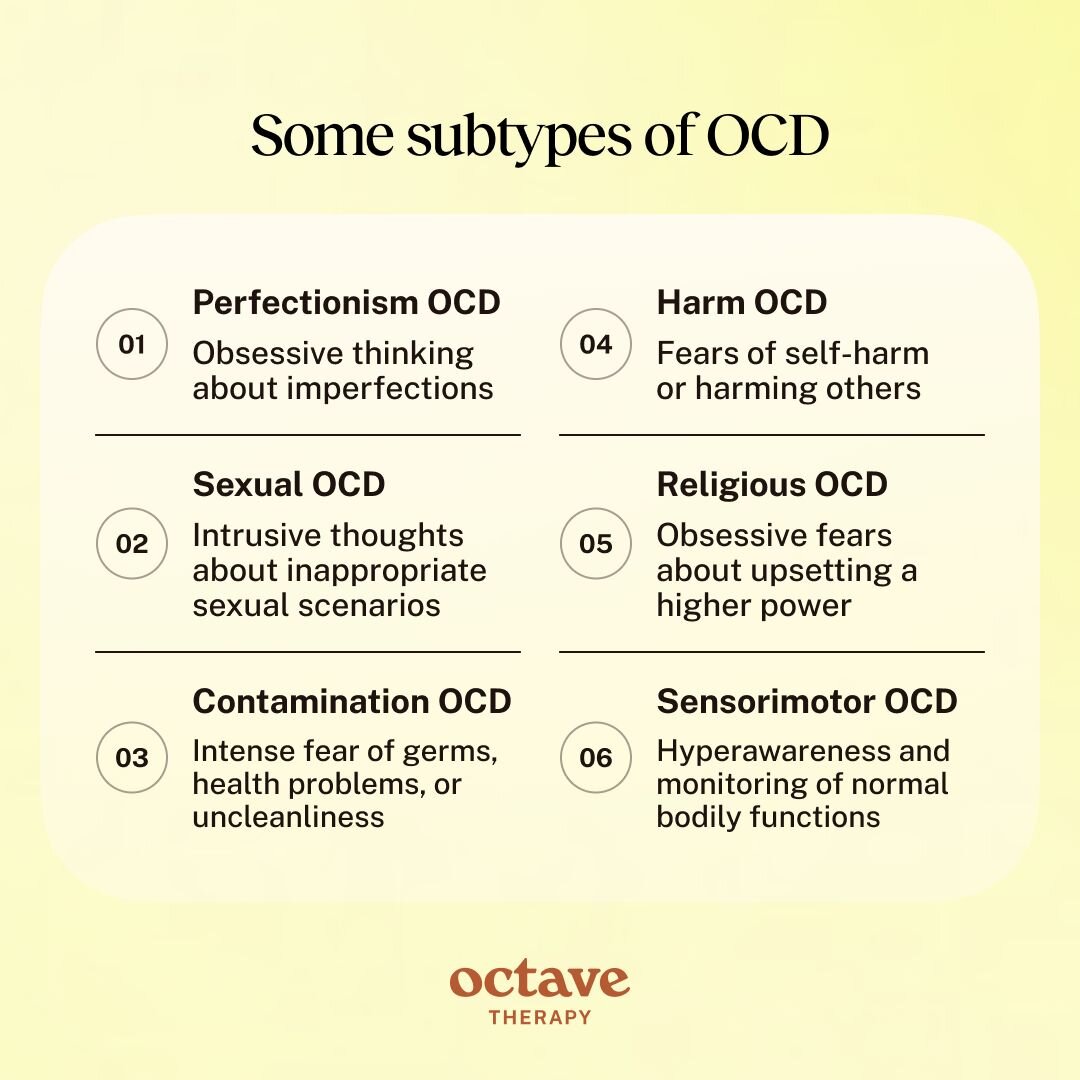
Types of OCD
There are many subtypes of OCD, each associated with specific kinds of obsessions and compulsions. These include (but are not limited to):
- Perfectionism OCD: Obsessive thinking about imperfections, leading to compulsions to do things in the “perfect” way. The person checks for errors in the work or responsibilities they’ve carried out, feeling intense anxiety that they have made mistakes.
- Sexual OCD: Intrusive thoughts or mental images about inappropriate, taboo, or harmful sexual scenarios. These thoughts are unwanted and lead to compulsions such as self-testing of arousal, reassurance-seeking, confessions, rumination, and attempts at suppression.
- Contamination OCD: Intense fear of germs, poor hygiene, health problems, and uncleanliness. Compulsions include the need to wash and clean excessively and to avoid situations where one might be exposed to a perceived contaminant.
- Religious OCD: Obsessive fears about sinning, immorality, upsetting a higher power, or heretical thoughts. The person feels compelled to pray, confess their sins, ask for forgiveness, or perform ritualistic acts.
- Sensorimotor OCD: The person is hyperaware of bodily functions like breathing, blinking, or swallowing, leading to compulsions to monitor and “correct” them.
- Harm OCD: Intrusive fears of self-harm or causing harm to others, commonly leading to compulsions to analyze memories, excessively seek reassurance, or avoid scenarios where they think they could cause harm.
Is OCD Common?
OCD is the fourth most common mental illness in the United States and around the world. Globally, OCD affects about 1% of the population. In the U.S., approximately 1.2% of adults suffer from OCD annually, amounting to roughly 3 million individuals. However, since OCD is often misdiagnosed, the number is likely higher.
People with OCD are at high risk of co-occurring mental health disorders, such as depression and anxiety, ADHD, and eating and substance use disorders.
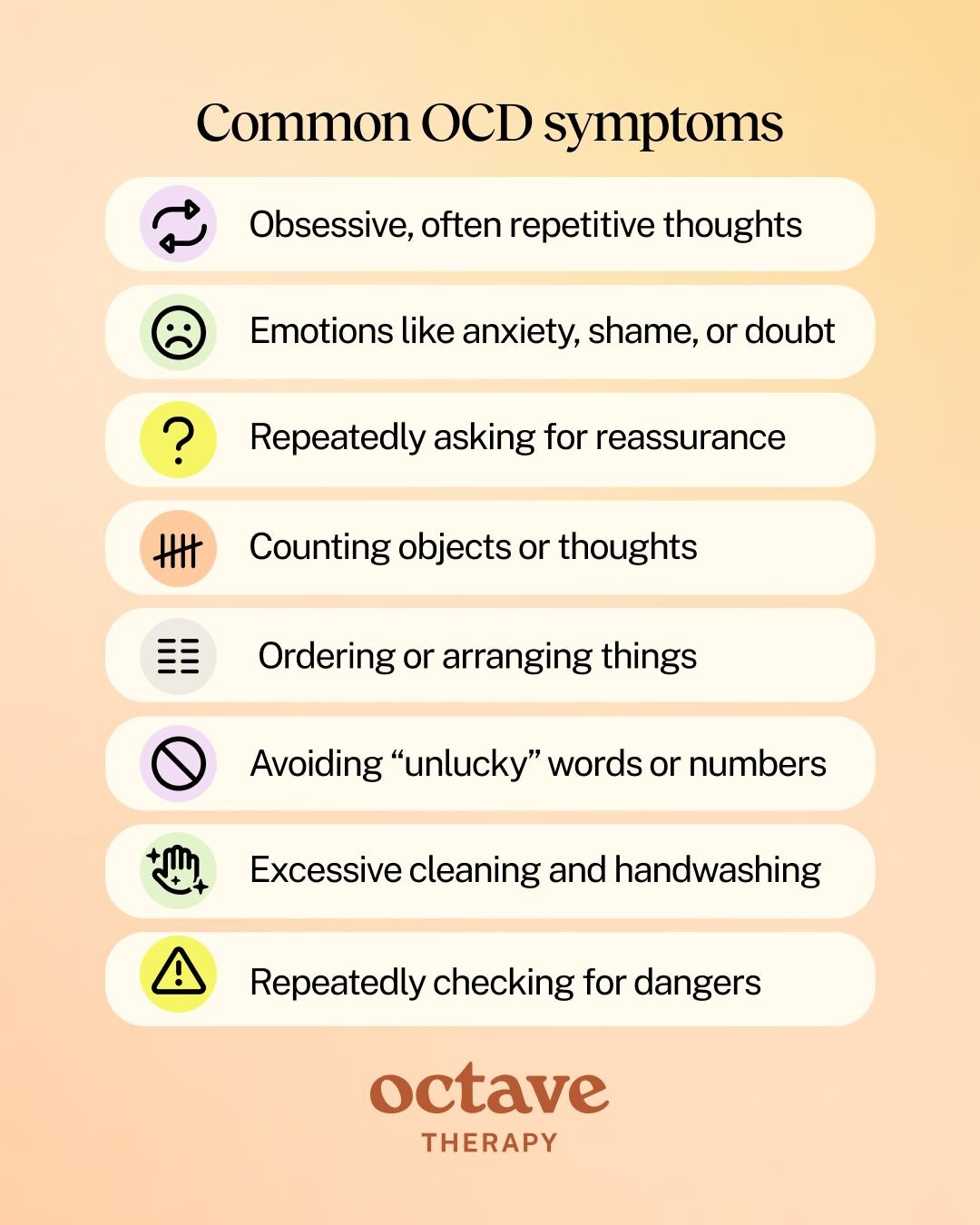
What are the Symptoms of Obsessive-Compulsive Disorder (OCD)?
The symptoms of OCD fall into three main categories: obsessions, emotional responses, and compulsions.
Obsessive Thoughts
Obsessive thoughts are distressing, intrusive thoughts, images, or urges that arise repeatedly in the person’s mind. Common obsessive thoughts include:
- Deliberately harming oneself or others through physical violence
- Accidentally harming oneself or others through mistakes such as leaving the stove on
- Becoming contaminated by disease, infection, or failures in hygiene
- Spreading contamination and causing illness in others
- The overwhelming need for symmetry or orderliness
- Potentially sinning or blaspheming
- Sexual taboos and inappropriate behavior
- Being sexually deviant
- Intense existential or philosophical concerns
- Flaws or infidelity in relationships
- The fear of certain words or numbers that are deemed “bad” or “unlucky”
Emotional Symptoms
The obsessive thoughts cause emotional distress, often leading to the following emotional symptoms:
- Anxiety and fear: the most common emotions experienced in response to obsessive thoughts, further driving those thoughts and compulsions
- Guilt and shame: especially for sexual and religious obsessions, even though the person does not act on them (and does not actually want to act on them)
- Frustration and irritability: stemming from the repeated interruptions of obsessive thoughts and compulsions in one’s life
- Helplessness and despair: regarding the persistent negative impact of obsessions on one’s functioning
- Depression and emotional exhaustion: the struggle to remain optimistic as the obsessive thoughts persistently drain one’s energy and prevent full engagement in life
- Uncertainty and doubt: the constant worry that something is wrong, leading the person to question their own experience and logic
- Numbness: the persistent intensity of emotions may lead to emotional blunting as a coping mechanism
- Social anxiety: whether caused by obsessions over relationships or fear that obsessions and compulsions will impact how people see the person
Compulsions
In response to the obsessions and their emotional impact, the person feels compelled to carry out actions that may provide temporary relief. Common compulsions include:
- Cleaning and hand-washing
- Repeatedly checking for mistakes or dangers
- Counting objects or thoughts
- Ordering and arranging items or behaviors
- Hoarding
- Asking for reassurance
- Mentally repeating words or phrases
- Thinking “neutralizing” thoughts to counter the obsessive thoughts
- Avoiding places and situations that could trigger obsessive thoughts
- Avoiding certain words or numbers that the person feels are “unlucky”
What Causes OCD?
There are a number of causes of OCD, including genetic, biological, environmental, and psychosocial factors.
Genetics
OCD has a strong genetic component, with research indicating that people with first-degree relatives (i.e., parents, siblings, or children) with OCD are up to 16 times as likely to develop it than the general population. Some specific genes, including genes that influence the production of neurotransmitters, have been identified as markers of a higher risk of OCD.
Brain Chemistry
Imbalances of neurotransmitters in the brain can contribute to the development and symptoms of OCD. In particular, low serotonin levels are associated with OCD.
Environment and Learned Behaviors
Environmental factors can contribute to the development of OCD. People who go through childhood trauma, including abuse, neglect, or loss of a loved one, are more vulnerable to developing OCD. This may be linked to the role of learned behaviors in causing the disorder.
For example, a person who experiences persistent parental neglect may become anxious about dangers like break-ins, house fires, and flooding. They start frequently checking locks, that heaters and ovens are switched off, and for leaks in the ceiling or basement. The behavior provides temporary relief from the anxiety and gradually becomes a compulsion.
OCD behaviors can also be learned from caregivers with OCD. A child who sees a parent engaging in compulsive behaviors to cope with anxiety may learn to use the same mechanisms, especially if the parent is also projecting or sharing their anxieties with the child.
Other Mental Health Conditions
Many (or even most) people with OCD have co-occurring mental health conditions, indicating that these conditions may contribute to its onset or exacerbate the symptoms. Common mental illnesses that co-occur with OCD include:
- Depression
- Anxiety
- Eating disorders
- Tic disorders or Tourette’s syndrome
OCD also commonly co-occurs with developmental disorders including attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD). Overlapping symptoms of these disorders with OCD can, however, complicate diagnosis.
Combination of Causes
The causes of OCD are not yet fully understood, and how it develops may vary from person to person. It is likely that, rather than one isolated cause, OCD is caused by a combination of heredity, biology, and environmental factors.
OCD Diagnosis
A person who is experiencing the symptoms of OCD can seek diagnosis from a licensed mental health professional, such as a clinical psychologist, psychiatrist, or therapist.
How is OCD Diagnosed?
When you or your mental healthcare provider thinks you may have OCD, they will conduct an interview, asking about your mental state and behaviors in order to check whether you have experienced various symptoms.
They may also inquire about your childhood and upbringing, looking for early signs of OCD and clues as to its potential causes, and ask for any information you have about mental health diagnoses within your family, as this might reveal a genetic predisposition to OCD and other mental illnesses.
Your therapist may also administer a diagnostic test that measures the symptoms of OCD and their severity. This can both improve the accuracy of the diagnosis and provide clarity on the right treatment plan for you.
Since OCD commonly co-occurs with other conditions, your provider may pick up on symptoms of additional mental illnesses or developmental disorders. In some cases, they may determine that your symptoms are caused by a condition other than OCD.
Criteria for an OCD Diagnosis
OCD must meet the following criteria in order to be diagnosed:
- Obsessions or compulsions or both are present
- Obsessions or compulsions are time-consuming, impede the person’s functioning, or are a source of distress
- The symptoms are not attributable to substance use or a medical condition
- Another mental health condition does not better explain the symptoms
The symptoms need to have been present on most days for at least two successive weeks.
Management and Treatment of OCD
Getting a diagnosis from your therapist or another mental healthcare professional is a great first step. Now, your therapist will collaborate with you and any other necessary mental health providers, usually including a psychiatrist, to develop a treatment plan.
Treatment for OCD generally consists of therapy and medication, often together with holistic or lifestyle recommendations that can improve your capabilities for managing OCD.
Medication for OCD
Certain medications can help with symptoms of OCD while also treating co-occurring mental illnesses like depression and anxiety. The most common medications prescribed for OCD include:
- SSRIs: these antidepressants are generally considered the first-line treatment for OCD. SSRIs increase available levels of serotonin, the deficiency of which is a hallmark of OCD.
- Clomipramine: a tricyclic antidepressant often used as a second-line treatment if SSRIs are not appropriate or effective. Clomipramine can have more severe side effects than other antidepressants, leading providers to be cautious about prescribing it.
- Augmenting medications: when the above medications are not effective or do not provide enough relief, providers may prescribe additional medications. These often include antipsychotics like quietapine (Seroquel) or glutamate-modulating drugs.
Therapy for OCD
While medications can provide relief for OCD symptoms, therapy is considered the most important treatment. In most cases, a combination of the two is used.
People with OCD respond particularly well to behavioral therapies, including:
- Cognitive-Behavioral Therapy (CBT): the techniques of CBT focus on identifying and changing problematic thoughts and behaviors and have had considerable success in treating OCD.
- Habit Reversal Training (HRT): for people with physical compulsions, such as picking skin, hair-pulling, or tapping, HRT trains alternative, non-harmful habits as replacements.
In severe cases of OCD that are non-responsive to behavioral therapies, deep brain stimulation is sometimes used. This uses a surgical procedure to place electrodes in the brain to regulate compulsive behaviors. While it is an evidence-based and FDA-approved treatment, deep brain stimulation is only used in extreme cases when other therapies are ineffective.
Exposure and response prevention is the primary CBT technique used for OCD. It works by gradually exposing the person to their obsessions while preventing them from acting on the associated compulsions. Starting with mild obsessions, the person learns to tolerate the thoughts and to not engage with them, or with the urges to act out compulsions.
For example, a person with with an obsessive fear of the number 13 might at some point in their treatment sit with a piece of paper with “13” written on it, looking at the number and noticing their urge to avoid it and the anxiety it provokes, while resisting the urge to engage in any compulsions. Over time, they learn that they can tolerate the anxiety the number evokes, and as a result, the anxiety lessens, and with successful treatment, the person no longer avoids the number.
What Should I Expect Living With OCD?
Living with untreated OCD can feel like being in a constant state of anxiety. It can be tough to control your mind, with distressing thoughts frequently arising, making it difficult to pay attention to your day-to-day life. Compulsions seem like the only way to get even temporary relief, but these activities can be as disruptive as the thoughts. They can also be harmful, whether physically or mentally.
If left untreated, OCD does not get better on its own. On the contrary, it tends to become worse, as the obsessions and compulsions get all the more overwhelming and exhausting.
Here are some issues people living with untreated OCD may experience:
- Co-occurring mental health conditions: The anxiety of living with OCD can itself become a separate disorder, as the person feels anxious even when not thinking obsessive thoughts. Depression is another common co-occurring disorder, triggered by the overwhelming flood of emotions that one experiences every day, leading to numbness, exhaustion, and despair.
- Isolation: Engaging with others socially can be difficult when living with OCD, as obsessions can at times make it difficult to focus on conversations or the needs of others, and compulsions cause disruptions and, all too often, shame.
- Academic struggles: With so much cognitive energy going towards obsessive thoughts, and time spent acting out compulsions, focusing on academics can become extremely challenging.
- Work struggles: Similarly, it can become difficult to function as effectively at work, with the intrusion of obsessive thoughts and time-consuming compulsions.
- Substance abuse: Substance use disorders commonly co-occur with OCD, as the person looks for a way to numb or escape from obsessive thoughts.
- Suicidal thoughts: People with Harm OCD experience obsessive thoughts about self-harm and suicide, even when they have no intention to act on those thoughts. For others, the mental health struggles caused by OCD can lead to suicidal thoughts.
- Time consumption: Compulsions can be time-consuming, especially when they are carried out multiple times throughout the day.
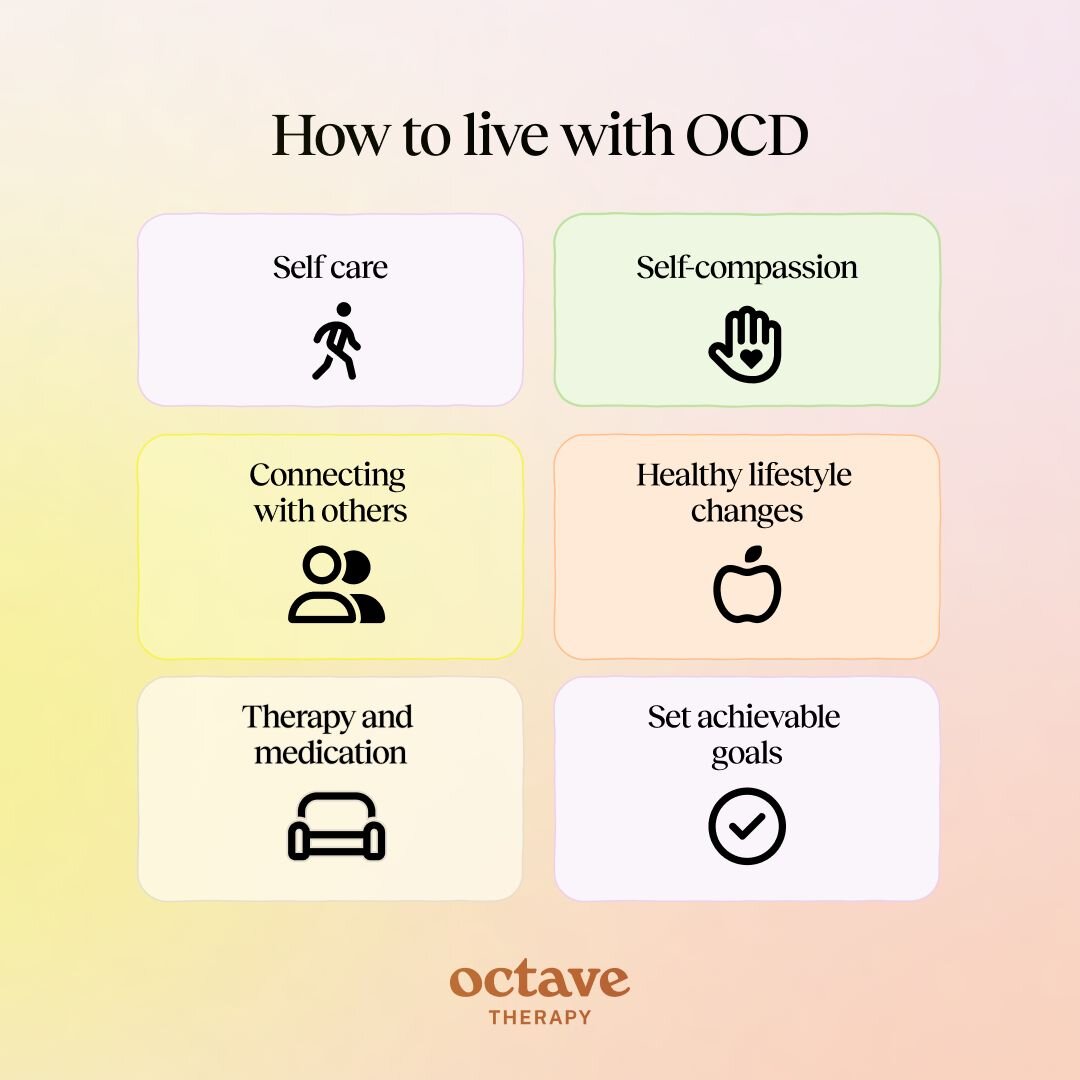
How to Live With OCD
In addition to therapy and medication, there are lifestyle changes that can help you live with OCD. These can also be helpful when you are still in the process of seeking treatment or in the early stages.
The following practices may help you manage life with OCD:
- Self-care: It is important to take time to do soothing or pleasurable activities that improve your wellness. These can include time spent in nature, warm baths, favorite meals, reading, listening to relaxing music, massages, and much more.
- Connecting with others: Isolation can be a consequence of OCD and can further exacerbate the symptoms. Remember to connect with loved ones you trust. Joining support groups with others who are diagnosed with OCD is another great way to help you feel less alone.
- Healthy lifestyle changes: Pay attention to how the things you do on a daily basis impact your mood and energy levels. You may find, for example, that minimizing time spent on social media helps to reduce overall anxiety levels. Similarly, notice if certain foods or substances, such as caffeine, exacerbate anxiety, and consider reducing or eliminating them. Getting regular exercise, prioritizing sleep, and doing your best to eat a nutritious diet are all habits that can help you maintain greater emotional balance.
- Self-compassion and patience: Living with OCD is difficult, but many people still judge themselves for their struggles. Practice self-compassion and be patient with your progress, keeping in mind that mental illness is not a weakness.
- Set achievable goals: OCD can be quite disruptive to one’s life, and it can feel like you are stuck sometimes. Setting achievable goals, even if they are baby steps, helps you to start gaining momentum.
When to Seek Help for OCD
If you think you have OCD and are wondering whether you should seek help, the answer is probably yes. When what seem to be the symptoms of OCD are affecting your happiness in your day-to-day life, seeking a diagnosis and treatment is crucial. You do not have to wait until it gets worse. In fact, the sooner you start treatment, the better.
Even if you do not receive an OCD diagnosis, seeing a therapist can help you manage the issues that are causing you distress. Therapy is a highly effective treatment for various mental health conditions, as well as for helping many people manage common life challenges.
If you are experiencing one or more of the symptoms of OCD, or are simply seeking a happier, healthier life, reach out to a mental health provider.